Yes. Radiofrequency ablation is a well-established drug-free treatment that has been clinically proven to provide safe, effective, lasting relief from your chronic pain.1,2 Talk with your doctor to learn more about the safety and effectiveness of Radiofrequency ablation.
Is RFA right for me?
Radiofrequency ablation can target pain in multiple parts of your body. If you have pain in more than one area, your doctor can address them all in a single treatment.
- Neck
- Shoulder
- Back
- Lower back
- Hips
- S.I. joint
- Leg
- Knee
- Foot
A pain management specialist can tell you if RFA therapy may be right for you. See the complete RFA indications and contraindications.
Have you been suffering from pain for more than 6 months?
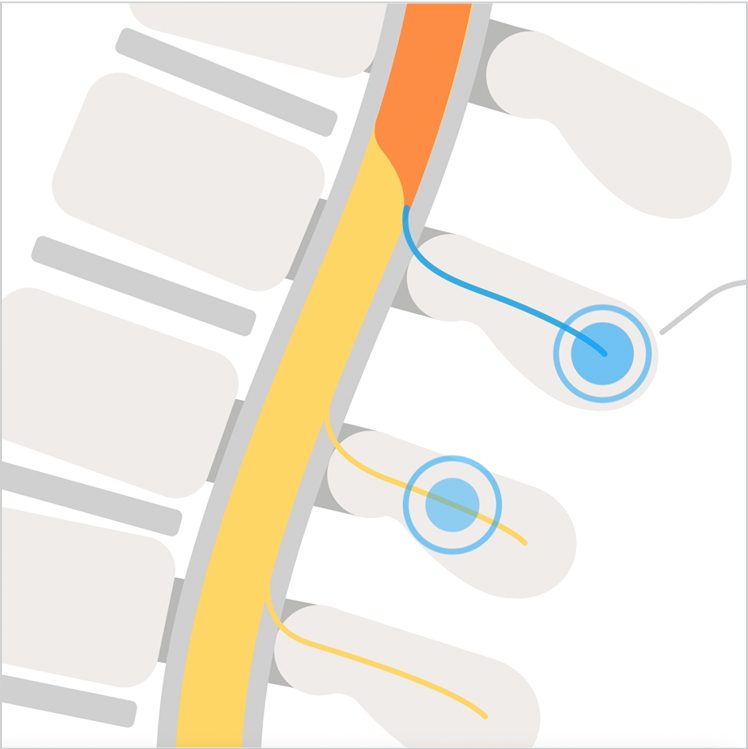
How does RFA work?
RFA is a simple, minimally invasive outpatient procedure. Your pain specialist uses radio waves to disable nerves transmitting pain signals, effectively interrupting those signals at their source.
See how RFA works
Watch this short, animated video to find out more about how RFA works and how it might help you find relief.
What to expect from RFA
As an outpatient procedure, RFA is a safe and minimally invasive way to treat certain types of pain. Here’s what you can expect before, during, and after RFA.

Preparing for RFA
To prepare for RFA, familiarize yourself with the procedure, including any fasting and medication guidelines provided by your healthcare provider.
On the day of your procedure, wear comfortable, easy-to-remove clothing. You’ll also need to ensure you have someone you can rely on to drive you home due to post-procedure drowsiness.

During RFA
On the day of your procedure, expect a quick, outpatient process. You will receive sedation and numbing to ensure your comfort during the treatment. Depending on the number of pain sources being treated, your procedure should last 20 to 45 minutes with a brief recovery period immediately following.
Afterward, plan to rest at home, arrange for help with responsibilities, and follow your healthcare provider's guidance for a smooth recovery.

Following RFA
For 24-48 hours after the procedure, you will need to rest and avoid driving or strenuous activity. You must follow any hygiene guidelines your doctor gives you, and you can manage any lingering discomfort with ice packs or prescribed pain relief.
Real-world results with RFA
Get the Radiofrequency Ablation brochure
Find the tools you need to take the next step towards lasting pain relief.
Frequently asked questions
Some insurance plans will cover radiofrequency ablation. Speak with your doctor and insurance carrier to verify.
The procedure is performed on an outpatient basis. Most patients are allowed to return home with few restrictions as soon as the effects of the local anesthesia dissipate.
RFA often results in meaningful pain relief for 6 months or longer. Some patients experience pain relief up to two years after their initial procedure.1,2
Your pain could return if the treated nerves regenerate. If this happens, the procedure can be repeated.
Take your next step toward pain relief
Have you been suffering from pain for more than 6 months?
References
- Provenzano DA, Holt B, Danko M, Atallah J, Iqbal M, Shah B, Singh A, Sachdeva H, Donck EV, Shaw E, Haas S, Sekhar R, Pan A, Halperin DS, Goldberg E. Assessment of real-world, prospective outcomes in patients treated with lumbar radiofrequency ablation for chronic pain (RAPID). Interv Pain Med. 2025 Apr 24;4(2):100576.
- David A. Provenzano, Bradley Holt, Michael Danko, Joseph Atallah, Maaz Iqbal, Binit Shah, Albert Singh, Harsh Sachdeva, Ella Ver Donck, Bart Liebrand, Erik Shaw, Sherri Haas, Rajat Sekhar, Ann Pan, Daniel S. Halperin, Edward Goldberg, Assessment of real-world, prospective outcomes in patients treated with cervical radiofrequency ablation for chronic pain (RAPID), Interventional Pain Medicine, Volume 4, Issue 3, 2025, 100623, ISSN 2772-5944, https://doi.org/10.1016/j.inpm.2025.100623.
- MacVicar J, Borowczyk JM, MacVicar AM, Loughnan BM, Bogduk N. Lumbar medial branch radiofrequency neurotomy in New Zealand. Pain Med. 2013;14(5):639-645. (N= 106)